Bilkul Sateek News
Process for obtaining financial assistance from the Chief Minister’s Relief Fund for medical treatment has been streamlined: applicants in need will receive aid within 15 days of applying.
Under the scheme, 25% of treatment costs—up to a maximum of ₹100,000—will be covered; each applicant may avail assistance only once per financial year.
Gurugram (Paridhi Dhasmana), April 25 – Deputy Commissioner Ajay Kumar announced that, in order to provide better healthcare services to the public, the Haryana government has introduced a simplified “SUKALP” portal for medical-need financial assistance from the Chief Minister’s Relief Fund (CMRF). The new system makes the application process faster and more user-friendly. Assistance amounts will be transferred directly into the applicant’s or beneficiary’s bank account.
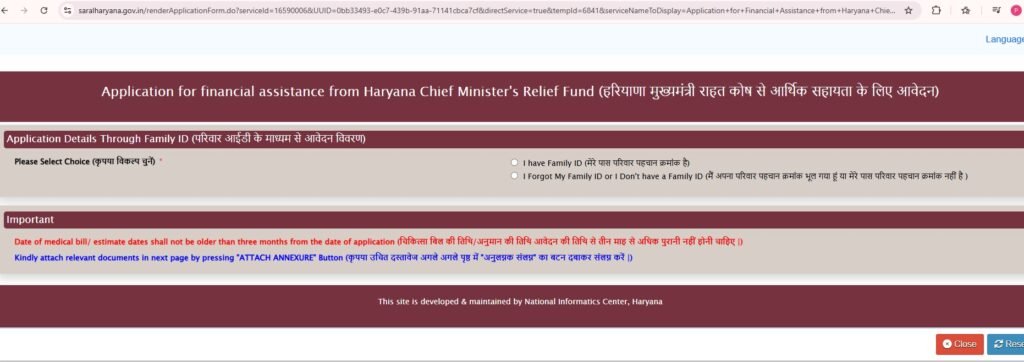
Applicants can apply via the SUKALP portal using their Family Identity Certificate (FIP) ID. To complete the process, they must upload relevant documents—such as medical bills and OPD receipts—and submit their CMRF medical assistance application online.
Under recent amendments, conditions or treatments not covered by the Ayushman Bharat–Pradhan Mantri Jan Arogya Yojana will now also qualify for CMRF aid, allowing even Ayushman beneficiaries to apply. A district-level committee has been constituted to oversee disbursements; its members include the local MP and MLA, the Deputy Commissioner, the Civil Surgeon, the chairs of municipal bodies and district and block councils, and the municipal commissioner as nodal officer.
The DC outlined the approval workflow: once an applicant submits their request, it is routed to the relevant MP, MLA, district council chair, block committee chair, and municipal head, who must forward their recommendations to the DC’s office within five days. The DC’s office then sends the application to the tehsildar for asset verification (four days) and to the Civil Surgeon for medical-document verification (five days). Reports from both offices are reviewed by the DC and the committee secretary, then forwarded to the Senior Accounts Officer for final sanction. Approved funds are directly credited to the beneficiary’s account.
Highlighting the inefficiencies of the previous system, the Deputy Commissioner noted that the revised process is both simpler and time-bound. He reiterated that aid will be directly transferred to the applicant’s or hospital’s bank account—if treatment is being received out of state, applicants may share hospital banking details to enable direct payment.
In summary, the scheme covers 25% of medical expenses (capped at ₹100,000), and each applicant may avail of the benefit only once per financial year.